Last week we ran a poll on Twitter to ask you if there should be a national standard for what constitutes a DNA; whether it's a patient missing an appointment or the patient cancelling their appointment on the day.
The debate began in our office when we realised that if a patient calls on the day of their appointment and cancels, some Trusts will consider this as a cancellation and some as a DNA. As insignificant as this may seem, it results in a huge discrepancy in the DNA rates across the country.
Traditionally, most Trusts use DNA rates as an indication of their financial performance. If Hospital A reports their DNA rate as 5% and Hospital B as 8.8% it would suggest Hospital A are performing better financially. This is as higher DNA rates are seen to indicate worse financial performance for a hospital. In reality, both of these hospitals may have the same clinic utilisation, so the difference in DNA rate does not indicate any difference in financial value. Without identifying the reason for empty appointment slots, a huge amount of unmeasured and unexplored productivity opportunity remains.
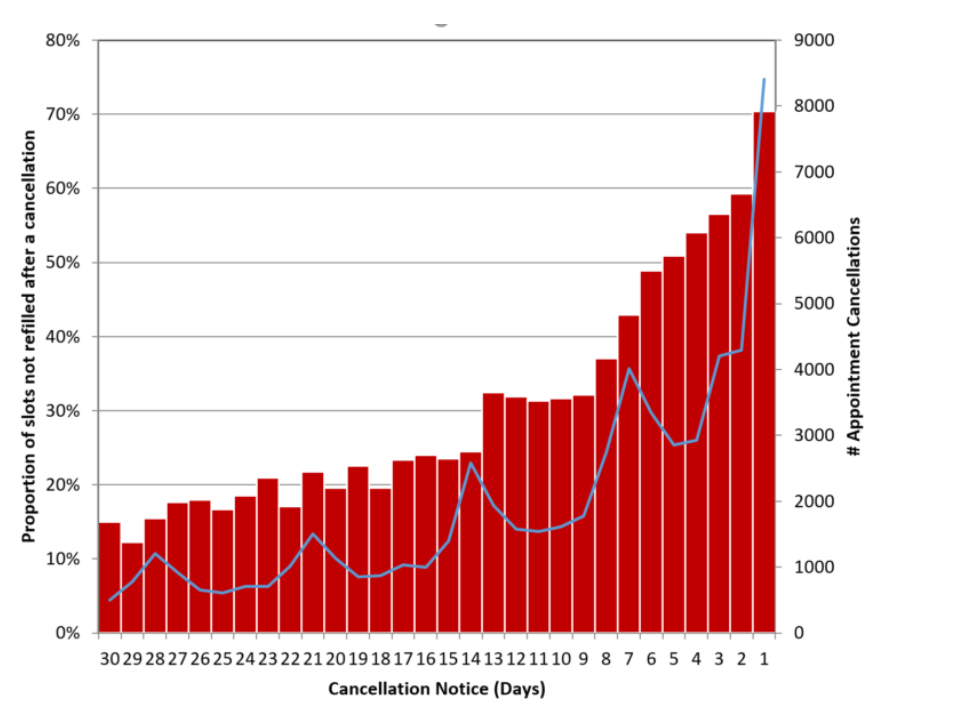
We conducted some research here at DrDoctor and found that most cancellations take place within 2 days of the appointment. If a cancellation occurs within 24 hours of the appointment date, 70% of those freed up appointments go unfilled.
DNAs have an enormous impact on the healthcare system in terms of cost and waiting time, significantly adding to delays along the patient pathway and increased patient dissatisfaction. According to the NHS Institute for Innovation and Improvement, the national DNA rate is over 10%.
The only major benefit of a last minute cancellation vs a DNA is that the clinician doesn’t have to wait around and can actively spend their time working on something else.
A DNA costs trusts between £90 – £140. For most acute hospitals, this is a multimillion pound problem and according to the NHS Information Centre there is a productivity opportunity of over £600 million based on average tariff by specialty by Trust.
In addition to financial impact, DNAs often present an additional negative consequence to patients. Patients who DNA are 40% more likely to present in A&E within the next 7 days, and one in 50 outpatients who miss an appointment fail to attend three or more further appointments within three months.
So why does it matter how we categorise these, if either way the slot doesn’t get used? In the case of cancellations, technology can come to our aid to refill slots quickly and automatically.
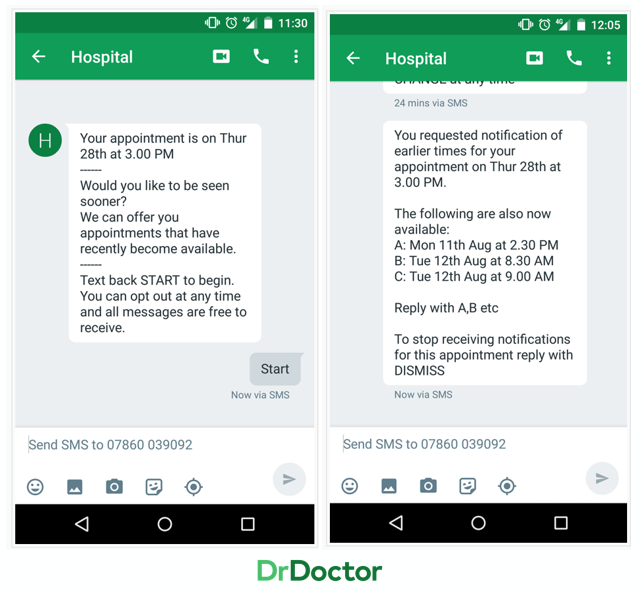
When a last-minute cancellation occurs, our See-Me-Sooner feature can offer the slot to a pool of patients, giving them the option to be seen sooner. The patient can choose to take the slot; reducing wait times and increasing clinic utilisation. Once accepted, their original appointment becomes free and that spot will then be automatically offered out to a pool of patients and the cycle continues. This allows clinics to run much closer to the capacity they were designed for.
Cancellations no longer go to waste and the automated systems can also reduce time on the phone by 50%. Reducing time spent cancelling and rebooking patients can be a huge cost saving measure.
So the question remains; should there be a standard definition for what makes cancellation and what makes a DNA, and does it matter? We think so and based on our Twitter poll, so do you!
With many important decisions resting on the back of metrics like these, it’s vital we see some consistency across the board. To get digital transformation right, hospitals need to accurately identify the potential in cancelled appointment slots. This is especially important when cancellations happen at late notice. Automation of refilling these appointments is an essential tool for increasing clinic utilisation but can only come from a place of clarity and accuracy.
