In October, we held an event with the Yorkshire & Humber AHSN and key figures in the field of digital health to explore the question; Digital-First NHS: Fallacy or Future?
This report covers the key takeaways from the day, which we hope will provide some shared learning for healthcare organisations in the north and beyond.
A special thank you to Paul Dimitiri of Sheffield Children’s NHS Foundation Trust, Richard Stubbs, CEO of Yorkshire & Humber AHSN and Graham Walsh of Calderdale and Huddersfield NHS Foundation Trust for speaking on the night and contributing to this report.
Download the full report here, including a foreword by Richard Stubbs.
Ensuring the future of a digital-first NHS
7 key stepping stones
1. Health inequalities
Technology has the potential to reduce health inequalities by enabling people to better manage their health and care through digital health information and tools. However, there is a digital divide and when we develop a technology we need to make it for the simplest use possible and work up.
It is also important to mitigate against digital health inequalities by addressing access and skills barriers and being aware of digital literacy. This can be achieved by involving users and tailoring services from the outset and also making sure that individuals are supported with improving their digital skills. As Richard Stubbs says “it needs to be baked in from the beginning”. Digital inclusion is not just about being online, it is also about building skills and confidence and in turn, willingness.
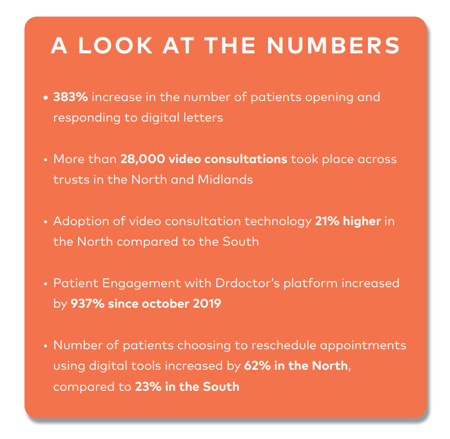
However, it’s not as black and white as it seems. The North, which is often associated with some of the widest health inequalities in the UK, has recently demonstrated higher digital adoption than the South. Our recent data shows that patients are becoming increasingly acceptant of a digital first NHS. Digital engagement has increased by as much as 383% compared to before the pandemic, with both clinicians and patients becoming more engaged and adopting these tools. This is likely to be because of the benefits of not having to travel to different hospitals.
2. prevention
Paul Dimitri, Professor of Child Health and Consultant in Paediatric Endocrinology, Sheffield Children’s NHS Foundation Trust, highlighted that a lot of health issues that manifest when we are 50, actually start in childhood.
He emphasised the need to invest more in children’s healthcare and technology, which is currently fragmented and poorly adopted, so that we are looking at how we keep them well.
Healthcare technology needs to be developed with patients to ensure it fits within the clinical pathway. We need to deliver healthcare in a different and exciting way for children to get the best education, for example by providing care outside of hospital and engaging them with technology.
Not all technology is likeable in healthcare and there are trust issues about who has developed this, how their data is being used and whether that technology is good enough.
3. Integration
Digital adoption is about integration – we need to develop the technology with healthcare professionals to enable it to be fit for purpose in where it needs to work. We need to create the right environment for digital technologies.
The challenge is making sure we don’t do a one size fits all approach. As Graham Walsh, Chief Clinical Information Officer at Calderdale and Huddersfield NHS Foundation Trust, highlighted it isn’t about replacing what NHS trusts are already doing with tech. He highlighted how post-operative wearables are being used with patients after knee surgery.
This means the surgeon can monitor how the patient is doing without the need for them to take time out of their day to attend a follow up appointment. Walsh highlights that the barrier is often the clinician – by developing technology with them we can get them on board from the outset. It needs to have a value for them to enable widespread digital adoption.
4. Devolution
We have probably all seen the regional inequalities in healthcare in different parts of the country. To do this there needs to be a shift to opportunity to level up health, between NHS services and social care, between physical and mental health, and between treatment and prevention.
Paul Dimitri, for example, highlighted that we need to level up investment in prevention for children and young people’s healthcare in a way that inspires innovation and technology-based healthcare for young people.
By doing this, young people would be heathier, our healthcare system would be less burdened, they would attend school more and society would be richer.
5. Culture of innovation
What we saw during the pandemic was a spread of innovation quickly and the breaking down of cultural barriers to adopting change. We now need to retain that momentum.
This can be achieved in a number of ways; by spreading the word between healthcare providers about what has already been done and by using AHSNs to work out where the warm conversations are. Relatively simple changes in behaviours and leadership processes can also have a great impact on the culture for innovation.
Healthcare providers need evidence that technology can deliver and mitigate risk. By engaging with them in this way and demonstrating what the tech does, rather than what it is, we can bring healthcare professionals with us.
6. Opportunity sits within the ICS
ICSs will enable flexibility for local areas to determine the best system arrangements for them. For ICSs to make the best use of technology, organisations need to work together to plan and invest in digital developments.
Digital innovations remain restricted to individual organisations, with limited shared learning or collaboration. This needs to be a joined-up approach so that once it is up a running in one area of the patch, it will trickle down to others.
7. Collaboration
There are increased levels of enthusiasm for digital products across the NHS, especially since the pandemic. AHSNs and NHSX are listening to suppliers to enable greater collaboration which will ultimately help to drive through change and execution in the NHS.
We need to re-look at how we deliver healthcare and we need to think about everyone together, especially with patients in mind.
Download the full report here, including a summary from DrDoctor CEO Tom Whicher.

